Health disparities were among the many challenges brought to the forefront during the COVID-19 pandemic. Recognizing COVID’s impact, the Centers for Disease Control and Prevention published a response outlining strategies to improve the health outcomes of populations disproportionately affected.[1]However, disparities and health equity are not new issues. Mandated by Congress and supported by a U.S. Department of Health and Human Services Interagency Work Group, the Agency for Healthcare Research and Quality (AHRQ) has reported on progress and opportunities for improving healthcare quality and reducing healthcare disparities for the past 17 years. Their 2019 National Healthcare Quality and Disparities Report encompasses reported patient care 2016-2018 and shows there are still disparities when comparing healthcare experience across races.[2]
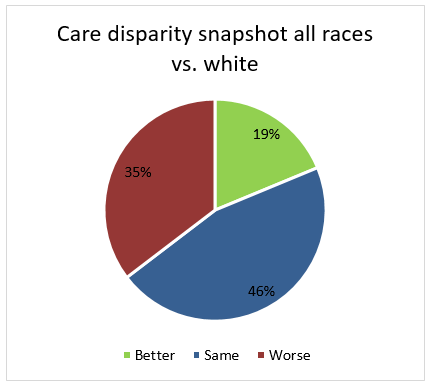
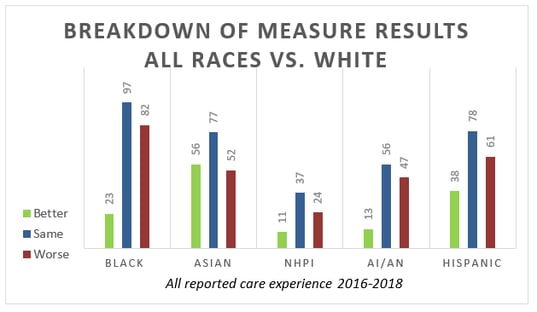
Between all reported races in comparison to whites, the report shows 141 measures where better care was received, 345 measures where the same care was received, and 266 measures where worse care was received.[3]
Note: the report also covers disparities for populations based on income stratification, level of insurance and residential demographics. We have elected to pull out the race data to coincide with the HEDIS measure specifications.
NCQA response includes a phased approach
The National Committee for Quality Assurance (NCQA) has stated that high-quality care is equitable care and there cannot be quality without equity. They are committed to building equity in all NCQA programs.[4]To help advance health equity, they will “play a primary role in driving the availability of standards and data necessary to identify disparities, enable positive change and measure outcomes.”[5]
Specifically, NCQA plans to enhance a variety of programs that span Health Plan Accreditation (HPA),[6] Multicultural Healthcare Distinction (MHC)[7] and the Healthcare Effectiveness Data and Information Set (HEDIS®[8])[9] in these areas:
- Identify and test standards that assess whether health plans have the structures and processes in place to help mitigate social risks and meet the health-related social needs of their members.
- Develop and test performance measures for plans that assess whether members are screened for health-related and broader social needs, as well as whether and how their social needs are met.
- Identify and test methods for assessing equity outcomes, such as developing benchmarks for equitable health outcomes for existing performance measures and examining approaches for using community-level outcomes for evaluating and incentivizing health plan performance.
NCQA developed a three-year phased approach for implementing race and ethnicity stratifications, with a stated goal of requiring all plans to report measure performance by race and ethnicity using directly collected member data by Measurement Year (MY) 2024. [10] For MY 2022, NCQA is requiring stratification by Race and Ethnicity for a subset of HEDIS measures. Five measures will be stratified in MY 2022, with a minimum of 15 measures stratified by MY 2024.[11]The final measures span the Effectiveness of Care, Access to Care and Utilization domains.[12]
Focus on Data Remains Vital
Data collected from members through surveys and assessments or from enrollment information furnished by state Medicaid or federal agencies is considered direct data, the gold standard according to NCQA standards. Plans that have incomplete data through direct collection methods may use a reliable and valid method of indirect race and ethnicity assignment.[13]Two example methods for indirect data collection are:
- Bayesian Indirect Surname and Geocoding (BISG) Method
- Geographic Assignment at Census Tract Unit
These methods of the imputation of race and ethnicity have been validated for use at a population level (Note: this imputation would not be appropriate at the individual member level), and will provide a bridge to give plans time to implement processes for gathering race and ethnicity information from their members.
Although NCQA is taking promising steps to promote health equity, other organizations are also administrating change. Get our "Driving Change in Health Equity: A Focus for NCQA and Other Industry Stakeholders" report for a deeper dive into other industry efforts, including information on the CMS Health Equity Plan for Medicare, and details on state initiatives that mirror the policy goals of NCQA and CMS.
[1] https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/cdc-strategy.html
[2] https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html
[3] https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2019qdr-core-measures-disparities.pdf
[4] https://www.ncqa.org/wp-content/uploads/2021/06/2021-0622-Future-of-HEDIS.pdf?utm_medium=email&utm_campaign=web-hedis&utm_source=sf&utm_term=20210622
[5] https://www.ncqa.org/wp-content/uploads/2021/01/HealthEquity_NCQA-Recommendations-to-Biden-Transition_Web.pdf
[6] https://dev.ncqa.org/about-ncqa/contact-us/public-comments/health-equity-strategy-and-updates-to-health-plan-accreditation-2022-public-comment/
[7] https://www.ncqa.org/programs/health-plans/multicultural-health-care-mhc/
[8] HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA)
[9] https://www.ncqa.org/wp-content/uploads/2021/02/Future-of-HEDIS_Digital-Measures-and-Equity_20210224.pdf
[10] https://www.ncqa.org/wp-content/uploads/2021/02/All-Public-Comment-Materials.pdf
[11] https://www.ncqa.org/wp-content/uploads/2021/02/All-Public-Comment-Materials.pdf
[12] https://www.ncqa.org/wp-content/uploads/2021/02/Future-of-HEDIS_Digital-Measures-and-Equity_20210224.pdf
[13] https://www.ncqa.org/wp-content/uploads/2021/02/All-Public-Comment-Materials.pdf
[14] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6338295/pdf/HESR-54-13.pdf
[15] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2653886/pdf/hesr0043-1722.pdf
[16] https://www.ncqa.org/wp-content/uploads/2021/02/All-Public-Comment-Materials.pdf
[17] https://www.census.gov/programs-surveys/acs/microdata.html
Written by Amy Salls
Sr. Director, Revenue and Quality Analytics